Home
About Us
Resources
Pricing
Contact
Blog
Home
About Us
Resources
Pricing
Contact
Blog
Writing nursing SOAP notes is an essential skill for nursing professionals given that nurses are required to document patient care and assessment details accurately and efficiently. This guide provides a comprehensive overview of how to write effective nursing SOAP notes, complete with examples to help you get started.
Patient-reported symptoms
Observable measurements
Clinical analysis
Treatment strategy
SOAP Documentation
Room 204A • Admitted Today
A nursing soap note is a documentation written by nurses where they provide information obtained subjectively and objectively in patient assessment. With the information that is derived in soap charting, it is possible to diagnose underlying conditon and even make treatment recomendations.
A nursing soap notes example is provided that makes it possible to obtain insight into how one can write a good soap note. The example clearly identies various sections that make up a nursing soap note and the information that should be included in each section. The example is based on an actual patient case that makes it possible for readers to have clear insight into how they should go about in handling each section.
Descriptive details are also provided which is essential in facilitating learning based on what a nursing SOAP note is and critical writing guidelines. Insight into how one can obtain SOAP note writing services is also provided thus fully meeting needs readers may have.
Our soap note writers have a high level of expertise that will make it possible for learners to obtain insight into how a good soap note entails. Most importanly, the nursing soap note example below will provide all the important guidelines in charting.
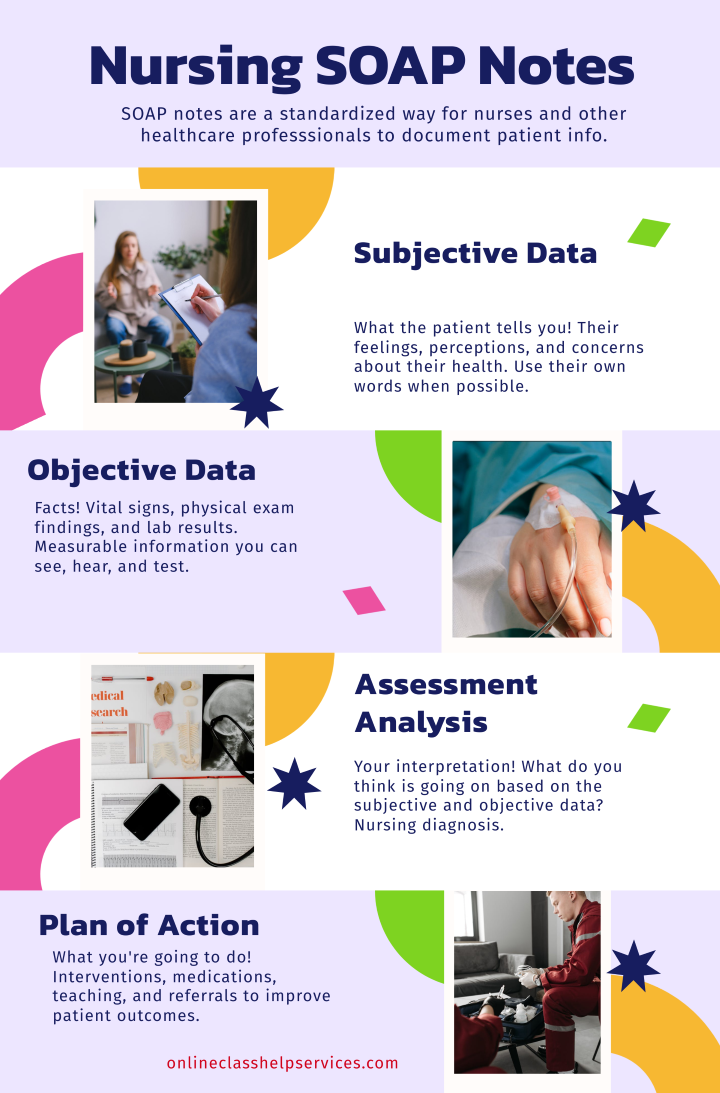
At first, it is important to understand what a SOAP note entails or to have clear insight into the definition of a SOAP note. The term SOAP usually comprises an acronym that stands for Subjective, Objective, Assessment, and Plan where each section has respective patient health information that should be recorded. The definition for a SOAP note is that it comprises a documentation used in patient assessment to help obtain and record information on underlying symptoms, patient’s medical history, and appropriate treatment recommendations.
According to Wiki How, each of the four sections must be completed with entirety that is critical in diagnosing the underlying condition and even coming up with an effective treatment plan. Each of the four sections will be covered and the information that should be presented in each section clearly illustrated.
Emphasis has made in this article on how to engage in nursing soap charting where an elaborate example is provided along with writing guidelines. With the derived insight, nurses will be in a position to undertake assessments on patients and even come up with effective treatment plans.
Nursing soap charting usually entails the process of writing a SOAP documentation upon the assessment of underlying patient condition. As a nurse, you are going to be required to come up with a SOAP note at some point in your career or learning. It is important for you to understand the guidelines that you should apply as you engage in SOAP charting. The example that we have provided and discussed extensively below clearly illustrates the SOAP note format that should be applied in charting.
Our soap note writer applies the format that is captured in the sample and the format is also standard for all documentation. Therefore, if you are experiencing difficulties in undertaking your assessment, you can understand how you can come up with subjective, objective, assessment, and plan sections. The nursing soap charting example below will place you at a better position for writing a perfect documentation.
The following is a nursing soap note example where the information that should be included in each section has been discussed and identified. This example is based on an actual patient case that makes it possible for readers to have clear insight into how they should go about in handling each section.
By considering the information provided in this example of a nursing soap note, it will be possible to come up with a soap note that meets required thresholds. This example has been prepared by our best soap note writer and it should not be copied for personal use.
CC: Family conflict
History of Present Illness (HPI): The patient in as immigrant who presents for a medical interview accompanied by her daughter aged 23 years and her therapist. She immigrated into the United States 12 years ago with her four children from Iran through a medical visa. One of her daughters that has accompanied her for the interview and who was aged 8 years at the time was left behind with her father in Iran. However, the father abused her emotionally, physically, and sexually before she later moved into the US to live with her mother 2 years ago. The mother has completely separated from her husband but has a history of domestic abuse from the marriage. Currently, the mother is disabled following a failed leg surgery that has rendered her inactive and made it impossible for her to work or even to operate independently. The main reason why the mother and daughter went for therapy is as a result of family issues or conflict. The mother claims that her daughter has not been there for her to provide support and help. She currently explains that she had been depressed and that this daughter, rarely spends time with her despite not having a full-time job. On the other hand, the daughter indicates that she has a lot to do and that the mother has to learn living independently.
Past Psychiatric History:
Substance Current Use and History: No current or history of substance use.
Family Psychiatric/Substance Use History: Father has a history of smoking and alcohol abuse. However, the daughter has a history of emotional history following physical and emotional abuse from her father and current experienced with her mother (See appendix 1). Father was emotionally unstable and violent causing her to abuse his wife and children.
Psychosocial History: The mother is currently disabled and spends most of her time at home watching TV and performing simple chores such as cooking. She currently lives with two of her children and two pet dogs. She frequently visits her elder daughter who is married. She rarely interacts with other individual in her community or even engaging in social activities such as going out with friends. On the other hand, the daughter currently lives on her own but visits her mother for a few hours in a week. She has no full-time job but is busy running errands to earn a living. She enjoys spending time with her friends especially during the weekends. She denies engaging in risky activities such as drug use.
Medical History:
Review of Symptoms (ROS):
Physical exam:
Diagnostic results:
Mental Status Examination: It is clear that both the mother and the daughter have unstable mental states that could be contributing to the underlying conflict. At first, the mother is stressed and depressed given the inability to function normally. On the other hand, there is a high likelihood that the daughter is highly stressed following the pressure that her mother is putting on her along with the effects of abuse in her childhood.
Differential Diagnoses:
Primary diagnosis: Mother: psychotic depression Daughter: Stress
Given the video presented, it is clear that the interviewer has facilitated the engagement between the mother, daughter, and the therapist in an excellent way. At first, the therapist has been used as an intermediary that has helped reveal details about the family given her time working with the mother. This has also helped to make the mother and daughter confident in sharing due to their trust to the therapist. Appropriate questions have been applied for the interview that have revealed details about what could be causing conflict between the mother and the daughter. Each individual is given appropriate time to present their argument without victimization. In such an encounter, I would employ a similar strategy where I would engage or involve the therapists that have dealt with members of the family to help establish trust.
Case Formulation:
Presenting complaint: Both the mother and daughter have presented for therapy following underlying differences that have made it almost for them to co-exist in peace.
Case presentation: Currently, the mother is disabled following a failed leg surgery that has rendered her inactive and made it impossible for her to work or even to operate independently. The main reason why the mother and daughter went for therapy is as a result of family issues or conflict. The mother claims that her daughter has not been there for her to provide support and help. She currently explains that she had been depressed and that this daughter, rarely spends time with her despite not having a full-time job. On the other hand, the daughter indicates that she has a lot to do and that the mother has to learn living independently.
Psychiatric symptom and diagnosis: It is clear that both the mother and the daughter have unstable mental states that could be contributing to the underlying conflict. At first, the mother is stressed and depressed given the inability to function normally. There is a high likelihood that the mother could be suffering from psychotic depression given that she confesses that she has depression and due to the constant pressure that she places on her daughter. She fails to acknowledge that her daughter is an adult buts puts pressure on her to visit her. She insists that things should go her way and fails to emphasize with her daughter who raises her concerns. The mother seems to have lost touch with the reality and given that she has depression, she is more likely to be suffering from psychotic depression. On the other hand, due to the pressure that the mother places on her daughter, she is more likely to be suffering from stress. This also explains why she seems to be avoiding her mother given that she presents as stressor.
Treatment Plan:
Having provided a detailed example of a nursing soap note, we are going to discuss information on the details that should be included in each section. This will make the feedback provided clearer and also offer insight into how to write a good soap note.
This section of the SOAP note usually requires an individual to provide information regarding the conditions that may be underlying in the patient. For instance, a patient may be presenting for a mental health assessment where brief information regarding mental health assessment can be discussed. One can also provide general information regarding a patient’s health.
This is the first section of a nursing SOAP note where one has to provide information regarding the patient health and social history. The information that is obtained in this section is very important since it makes it possible to understand the condition that is underlying in the patient. At first, one must begin by identifying the chief complaint which is the main issue that is presented in the patient as seen in the soap note example above.
The information that is featured in the subjective section of a nursing SOAP notes usually comprises the information that a patient shares regarding their health. As illustrated in the nursing soap notes example, one should provide details about history of present ilnesses (HPI) after identifying the chief complain. This should be followed by information about the past pyschiatric history, family history, and substance use history. These details can be very signficant in the diagnosis of underlying conditions and should not be left out.
While coming up with a nursing SOAP notes, one usually provides their own perception regarding the symptoms that are presented in the patient. Generally, one usually provides information based on the question they ask the patient and even what they observe. The objective section should comprise information that the healthcare professional identifies as they assess a patient. Details about vital signs should be provided where information on signs such as temperature and blood pressure are provided.
As exhibited in the nursing soap notes example above, one should begin by providing information obtained through physical assessment. Details that are similar to those provided in the objective section are provided but the information is based on what a healthcare professionals identified. For instance, one must provide information about the review of symptoms (ROS) which is also provided in the subjective part.
This section of a nursing SOAP note requires you to provide details regarding various conditions that have to be considered for differential diagnosis. Various conditions that are considered for diagnosis are listed and a primary diagnosis selected. With the information obtained upon assessment, it can be possible for a competent healthcare professional to decide on the conditions that a patient is likely to be suffering from.
Various probable underlying conditions should be included in the assessment section of a nursing soap note in the order the conditions are likely to be affecting the patient. With this insight, one should the select the condition that has a high likelihood of affecting the patient. The nursing soap notes example we have provided clearly shows how the conditions should be identified and even how a primary diagnosis should be illustrated.
This section is important since it provides guidelines based on the activities that have to be undertaken to promote recovery in the patient. To effectively come up with this part, one must ensure that they diagnose the underlying condition with clarity. The plan section of a nursing SOAP note usually identifies various directives that should be undertaken in treatment. The medications that are best suited to addressing the underlying condition should be identified in this part.
Other details that should be included in the plan section comprise information on follow-up and patient management practices. It is important to include details about when a patient should return for follow-up and even the practices that they should take to promote recovery. These directives are very critical in enabling the patients and home-based care givers undertake approriate care practices. Additionally, a good SOAP note should also have a reflection section and a conclusion section.
The reflection is very important for one’s professional growth and even for the wellbeing of the patient. While coming up with a reflection, one should ensure that they provide their thoughts regarding the lessons learned and even what they may have observed or even thoughts elicited. While writing the reflection section of a nursing SOAP note, one also has to capture information regarding how the lesson learned can influence their future practice. It can also be crucial to provide details about the new ideas that came up based on activities undertaken in assessment. You can obtain guidance from the best soap note writer that will enable you write a good reflection in case you are experiencing any difficulties.
This section helps to bring closure to the nursing SOAP notes where one provides a summary of the main issues that came up and the actions that were taken. When writing a conclusion, you can briefly identify the condition diagnosed and even the proposed treatment guidelines. Additionally, it is important to include a list of sources that were used in providing the information discussed. You can chat with a SOAP note writer that will enable you come up with a good conclusion thus meeting all important requirements for your documentation.
If you are struggling with writing your nursing SOAP notes you can obtain soap note writing services that will enable you come up with a good documentation. We have the best soap note writers and therefore, do not hesitate to reach out to us for any writing support. The soap note example that is provide offers proof that our experts have clear insight into how to come up with a good documentation.
Therefore, if you need nursing soap notes essay help, you can simply place an order for your essay. Simply follow the ordering process and provide us with details on your essay. Alternatively, you start a chat with us where we can guide you on how go about in placing your order. You can apply the nursing soap notes example provided in conducting assessments or seek help from our soap note writers.
Connect with our expert writers for professional academic assistance.