Home
About Us
Resources
Pricing
Contact
Blog
Home
About Us
Resources
Pricing
Contact
Blog
Master the art of writing Nurse practitioner SOAP notes with our comprehensive guide and example tailored for Nurse Practitioners. The following guide and examples will help you create effective SOAP notes that enhance patient care.
Patient history & symptoms
Clinical observations
Clinical diagnosis
Treatment strategy
SOAP Note System
A nurse practitioner soap notes usually entails a documentation that is used in advanced practice by nurses to help assess and diagnose patient. The acronym ‘SOAP,’ usually stands for Subjective, Objective, Assessment, and Plan where each part has specific details that should be provided.
We are going to discuss that should be provided under each part of a NP SOAP note. The details should be provided in a chronological order, where information should flow starting from when the assessment is conducted to when a treatment recommendation is made.
To promote a proper understanding of the essential details, a nurse practitioner soap notes example has been provided. Each section has been clearly identified along with the information that should be included in each part of the soap note.
The example can be applied in SOAP charting aimed at facilitating learning or even for professional purposes. Additionally, directives one how one can obtain expert help are provided at the end.
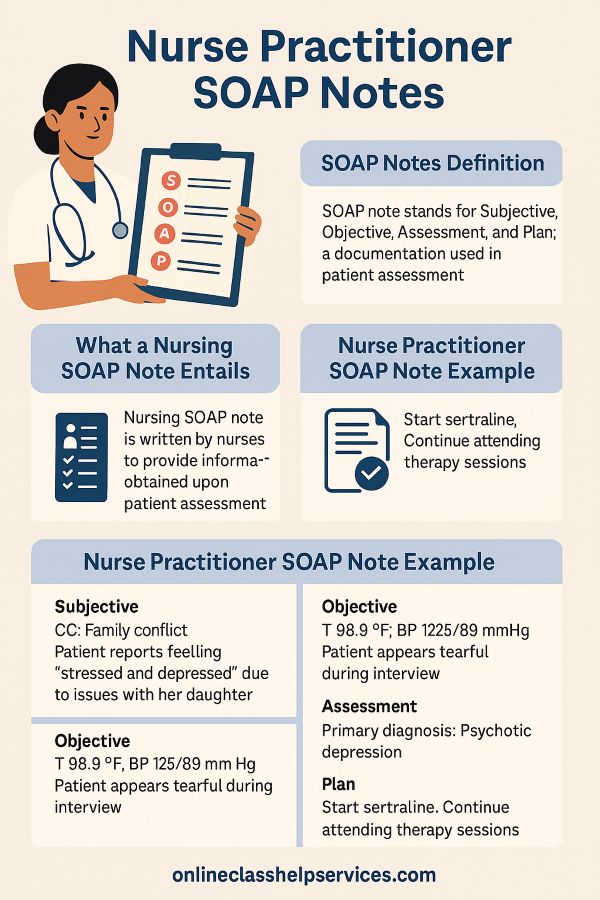
This is an example of a nurse practitioner SOAP note where the information that should be provided in Subjective, Objective, Assessment, and Plan sections have been provided. The example is based on assessment of a patient that has an underlying mental health disorder. To ensure that well-informed details are provided, a real patient-case scenario has been provided. Therefore, you can simply go through the NP SOAP note example to obtain insight into how you can engage in SOAP charting.
Sudden feeling of a racing heartbeat, sweating, and shortness of breath.
Mr. T.P is an 18-year-old Caucasian male who presents for assessment and treatment. Based on the feedback provided, the patient has been experiencing sudden feelings of a racing heart that is accompanied by sweating and shortness of breath. This feeling has been recurring over various days where each incidence usually lasts for 15 minutes. The feeling occurs unexpectedly given that at one time, it happened while he was making coffee. No medication has been administered at the moment.
The patient has no history of any psychiatric condition or disorder.
The patient denies the use of drugs or alcohol.
18-year-old Caucasian male who currently a local community college for graphic design. He currently in a relationship with his girlfriend in high school. The patient is neatly dressed with well-kept hair. He maintains coherent and articulate speech. He does not appear tired or withdrawn from conditions such as drug use. The patient appears distressed and worried by his state of health.
Panic Disorder- There is a high likelihood that the patient could be suffering from Panic-Disorder due to similarity in the signs expressed and those of the condition. However, with the proposed diagnostic tests, it will be possible to rule out anxiety attack and hyperthyroidism that will help reinforce this diagnosis.
Based on the case that has been presented, one obtains clear insight based on how a psychiatrist assessment can be conducted. At first, the nature of the assessment conducted is relevant where the examiner followed the required guidelines. At first, ethics such as respect and empathy that govern psychiatrist evaluation have been followed that is essential in making the patient feel comfortable (Coady, 2020). The examiner provides ample time to the patient to explain his condition without having to appear nagging and manipulative. Valid lead questions are used such as the instance where the examiner asks the patient where he had to go to the emergency department. Perhaps, one main lesson that has been drawn is that as a psychiatrist examiner, one must take time to carefully listen to the patient. This provides a basis for making decision based on the underlying case having obtained the relevant information.
Given the nurse practitioner SOAP note example that has been provided above, it is essential to provide readers with additional descriptive details based on each section. This will enable nursing professionals and learners required to write a SOAP note to obtain insight into how they can come up with a good SOAP note.
Any SOAP note has four main sections with each section providing different information with regarding to underlying patient condition. The details provided in each part are discussed as follows:
It is always good to start your NP SOAP note with an introduction part where you can provide generation information regarding a patient. For instance, if you are dealing with a patient with a mental health disorder, you can discuss general information regarding mental health disorders. You can also provide brief information regarding the patient that is being assessed. This part of your soap note sets a stage for the activities to be undertaken in assessment based on the four main parts.
The subjective part is the main part which is evident from the nurse practitioner SOAP note example above. The information provided in this part usually comprises details that a patient shares regarding how they are feeling. Generally, the information regarding the patient’s health history and current symptoms is provided. At first, one must identify the chief complaint after which they should provide details about the history of present illness (HPI).
Details about the psychosocial history, substance use history, and family history must also be provided in this part. The details on each of the component have been clearly indicated in the nurse practitioner soap note example above. A review of symptoms (ROS) should also be provided along with details on the medical history. For further insight into the information that should be provided, you can review the example provided above.
The objective section of a nurse practitioner SOAP notes is the second section and one should begin by conducting a physical exam on the patient. Details that are provided based on the Review of symptoms in the subjective part should also be provided in this part. However, for this part, the details must be based on assessment undertaken on the patient by the healthcare professional.
Details about diagnostic results should also be provided which includes the information that derived from tests conducted on the patient. The respective test that is used in assessing the patient should be identified. With the example that is featured above, one can identify the information that professionals should provide and the required order.
For this part, one majorly provides details on the conditions that are considered for differential diagnosis. With the information that is obtained in the first two parts of a nurse practitioner soap note, it can be possible to determine the underlying patient condition. As a healthcare professional, one can be in a position to associate the symptoms identified with various illnesses.
The illnesses that are considered for differential diagnosis should be identified and a primary diagnosis identified. The various conditions considered are usually identified starting with the condition that the patient is most likely suffering from. Other probable conditions are also identified as illustrated in the nurse practitioner SOAP notes example above. Lastly, one should then identify the condition that should be considered for primary diagnosis.
For this part, one has to come up with a treatment plan based on the condition that is diagnosed. The treatment plan comprises the patient care, medication, and management guidelines that should be followed. The example provided above does not include a treatment plan but you can check out our nursing SOAP note example to obtain insight into how this section should appear.
Details about the medication that the patients should take should be provided in this section. It is also important to offer guidelines on actions that a patient should take to promote follow-up. Apart from the four main sections, there are two additional components that should be included to come up with a complete nurse practitioner SOAP note. This includes the reflection and the conclusion parts that are discussed as follows.
For this part, you should share information about thoughts that came up as you were engaging in the entire assessment process. For instance, you can provide information regarding the new ideas that came to mind. You can also provide information regarding new details learned and how you will address similar situations better in future. The nurse practitioner soap notes example featured has clear details on information that should be included in the reflection part.
This is the last part of a nurse practitioner SOAP note and it is similar to the conclusion provide in other research and academic papers. A brief summary of all the details provided in the documentation are provided in this part. The conclusion should give your documentation closure while showing that the patient’s needs have fully been met. Lastly, it can be necessary to include references to support the information provided. Therefore, with the details that this article provides, it can be possible to come up with a NP SOAP notes that meets required Guidelines.
With the details above, it can be possible to undertake an assessment on a patient and even come up with a documentation that has all sections. However, it is normal to encounter difficulties in SOAP charting where it is preferrable to reach out to experts for help. This can hinder the ability to undertake the required activities in charting thus limiting the desired treatment outcomes.
With the guidance that is provide by our experts, it can be possible to engage in SOAP charting with ease. We have a high level of expertise thus making it possible to provide guidance, help, and even consultive services at a high reliabiliy level. Therefore, simply contact us or feel free to apply the nurse practitioner SOAP note example above in charting.
Connect with our expert writers for professional academic assistance.